COVID-19 taught the healthcare industry that a room inside a hospital can’t serve just one function. But even emergency departments aren’t capable of everything — not yet.
Providers had to toss the standard playbook in the outset of the pandemic. If healthcare facilities are to inspire a sense of calm in the midst of chaos, they will need to be even more resilient and adaptable to coordinate departments during mass emergencies.
The need is especially acute in emergency departments, where stakes are often highest. Hospital leaders and builders must work together to create more adaptable spaces that can accommodate different systems and types of patient care so they can handle whatever may come their way.
COVID challenges: novel problems in existing systems
The COVID-19 pandemic presented a wide array of challenges not faced by the nation’s healthcare sector in a century.
A ventilator shortage in early 2020 put the healthcare industry on red alert as medical staff around the world scrambled to care for as many patients as possible with the limited amount of equipment fit for the challenge.
The rapid influx of highly infectious patients had traditional hospital systems bursting at the seams and potentially unable to cope with the patient care demands while maintaining staff and patient safety standards.
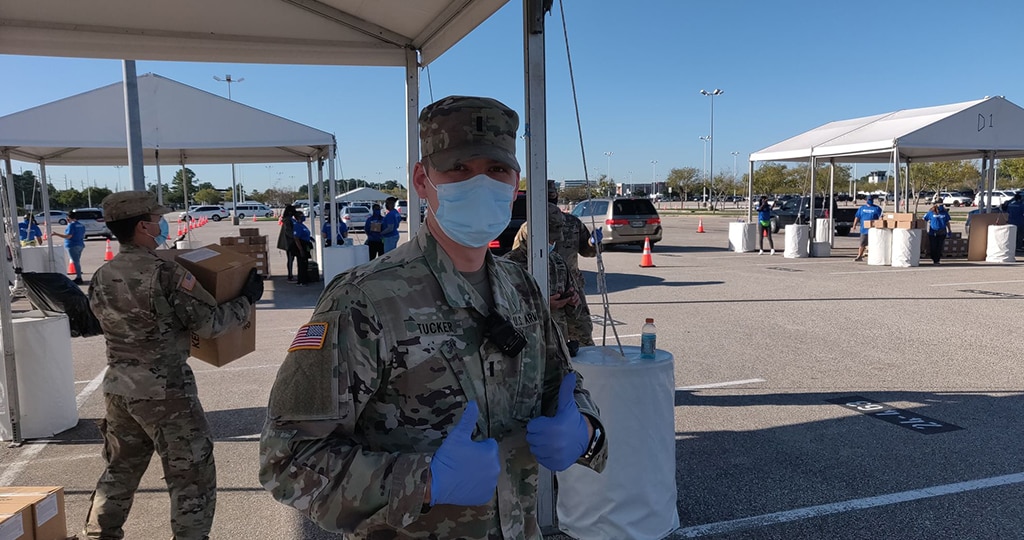
Medical and patient care staff members in urban and suburban areas required huge volumes of personal protective equipment (masks, gowns, gloves, face shields, etc.). Suddenly, crowded hallways were repurposed into multipurpose storage and even patient care spaces.
Existing air handling systems were not designed for the volume of patients requiring respiratory isolation and this simply exacerbated logistical problems and contamination risks.
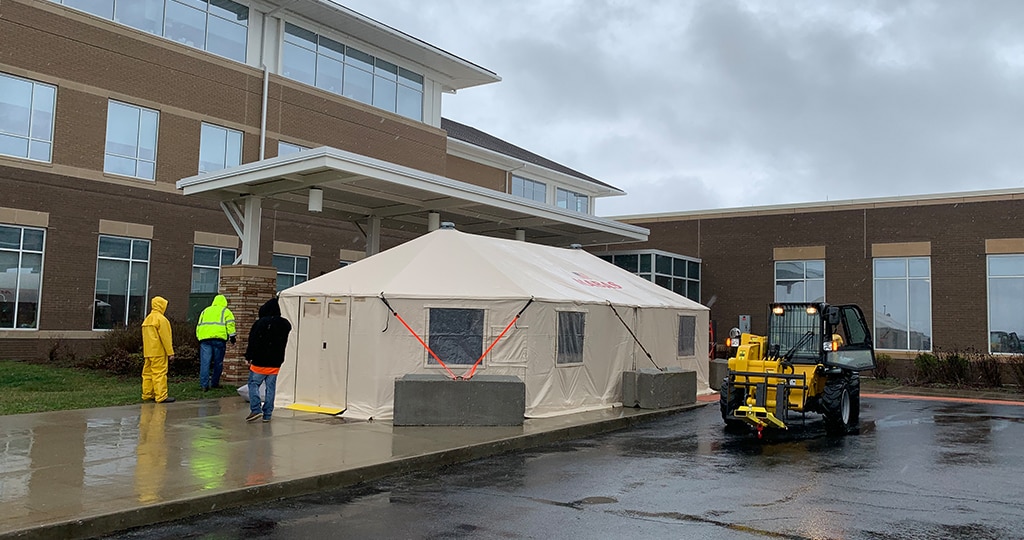
Hospitals in suburban and urban areas erected circus-size outdoor canopies and conference rooms were converted to handle overflow patient volumes. Pop-up tents and even garden sheds were used to screen and register potentially infectious patients in rural areas in an effort to segregate these patients from the general public and other patients requiring hospital services.
But after the initial wave, patient volume drastically declined for many emergency departments as potential patients avoided what the media suggested were contagion hotspots.
Major hospitals once required massive waiting rooms to house dozens of soon-to-be patients. But those crowded spaces became the antithesis of disease prevention. All those chairs sat empty as patients visited without accompaniment, put off elective procedures or turned to telehealth for checkups.
Wayfinding took on new importance as patients seeking emergency care feared a wrong turn into the COVID ward. This was especially true for emergency department patients who were frightened and stressed by other ailments or feelings of isolation because their family and friends were not allowed to accompany them inside.
New solutions: building versatility
Wayfinding expanded and diversified
In many ways, the emergency department is the front door of the hospital. In fact, the emergency department begins in its parking lot.
It’s an easy place for the flow of patients and medical providers to bottleneck. It’s also the last place you want that to happen, as would-be patients invariably rub shoulders in and around the entrance of the ER before they’re processed and separated.
Large hospitals can be rearranged with multiple access points to set routes based on disease as well as destination. For example, potentially contagious patients park in an exclusive lot, walk into the ER from an isolated entrance and follow a path through the hospital that only they can access.
It’s always been difficult for new patients and visitors to navigate complicated settings like hospitals, especially if they’re frightened or confused or handicapped. For potentially contagious patients, it’s important that they don’t have the opportunity to inadvertently enter spaces with other patients.

That’s why visitors should see wayfinding indicators like maps, signs and color-coded lines before they enter the facility. These visible directions are best begun from entry into the hospital grounds where they can be directed their entire journey through the parking lots, grounds and facilities based on their needs (or in the case of COVID patients, their potentially infectious condition).
Some simple remedies for crowds of waiting patients could come from the dining sector.
Rather than sitting together in large rooms, people can stay in their parked cars and wait for a text update from the front desk. They can walk straight into their appointment and limit any time spent in shared spaces.
The challenge here is factoring the time patients who walk slowly could take to travel from their vehicle to the front desk.
Once inside, patients should fluidly flow through the process with as little time spent in lines, waiting rooms and other shared spaces as possible, like a host keeps people moving to and from their tables without crowding the lobby.
However, hospitals are a bit more complicated than a restaurant, and hospital staff and Design-Builders are still working with healthcare leaders to rethink hospital layouts and improve patient flow.
They’re also thinking of ways to make it easier for hospital staff and patients to maintain clean, safe environments, such as giving medical staff more personal workspace and increasing antimicrobial touchpoints.
But the price of real estate and construction or renovation is always a problem when trying to expand medical facilities, especially in urban areas.
This leaves builders and healthcare providers to wonder, “Do we need these large-scale parking lots, conference rooms and waiting areas, or could those spaces be reimagined in more flexible, modular ways?”
Ultra-flexible spaces
Builders and healthcare leaders are discussing best practices for preparing any room in the hospital to readily meet the demands of the moment. Unfortunately, many hospitals find that issues such as licensing, billing and the lack of universality of patient care staff can make this design solution unworkable.
Can an empty parking lot quickly become an active field hospital with the appropriate equipment and coordination? For decades, hospitals have practiced mass casualty drills and often the parking lot could be converted quickly.
Can every bed in a facility be equipped for a wide variety of patient care needs? This is not a solution if there are not appropriately trained staff to accommodate those specialty patients.
Can any ward immediately convert to an intensive care unit or quarantine space? Again, licensing, billing and staffing expertise are all issues that must be considered beyond simple construction.
There has been a focus on adding more single-patient rooms in hospitals to give patients more privacy. But in an emergency, these rooms could accommodate multiple patients, if properly equipped.
Ready-made quarantine spaces would benefit from negative air pressure systems to limit the spread of airborne communicable diseases. Negative pressure pulls germs from the ward, into the ventilation system where it’s captured by filters. Unfortunately, it’s a rare commodity, often limited to isolated parts of the hospital or one or two rooms per nursing unit.
Medical care providers don’t always have the luxury of choosing where a quarantine zone needs to be located.
Entire floors can be fairly easily made into potential negative pressure spaces. The tricky part is making every room a potential isolation chamber without affecting the rest of the ward. Builders are challenged to develop pressure systems that pressurize specific rooms, then switch to different rooms the next day.
This will require specialized ventilation systems running to every room, which is no small job. Yet many hospitals accomplished this quickly during the onset of the first COVID wave.
While adding technology such as ventilators would be a major investment for any hospital system, it could prove to be a priceless commodity in the event of another pandemic.
Many healthcare leaders wouldn’t have considered this a worthwhile investment at the beginning of 2020, but priorities drastically shifted over the course of the year, converting calculations from, “how much will it cost?” or how often will we ever use it, to “how many lives will be lost if we do not?”
Let’s get ready
As experienced healthcare builders, it’s our job to help healthcare leaders take advantage of what we’ve learned from this past year to make sure that the years to come are better for everyone.

If your hospital system is ready to work the numbers and find out the best way to become more flexible, reach out to our architectural design team and let’s reimagine what your facilities can be.
We’re experienced builders in the healthcare sector and are ready to help prepare your system for whatever challenges tomorrow may bring.
